Clinical Progress Notes Document Template
SOAP-format notes used to track a patient’s clinical progress during treatment.
Clinical Progress Notes
Purpose: These SOAP-format (Subjective, Objective, Assessment, Plan) notes are used to document a patient's clinical status, treatment progress, and plan of care across multiple visits. This format ensures consistency and clarity in medical records.
Patient Information
Name: {name}
Date of Birth: {dob}
Patient ID: {patientId}
Visit Date: {visitDate}
Clinician: {clinicianName}, {clinicianTitle}
Subjective
Chief Complaint: {chiefComplaint}
History of Present Illness: {presentIllness}
Patient Reported Symptoms: {symptoms}
Current Medications: {currentMedications}
Allergies: {allergies}
Objective
Vital Signs:
- Blood Pressure: {bloodPressure}
- Heart Rate: {heartRate}
- Respiratory Rate: {respiratoryRate}
- Temperature: {temperature}
- Oxygen Saturation: {oxygenSaturation}
Assessment
{clinicalAssessment}
Plan
Treatment Plan: {treatmentPlan}
Medications Prescribed: {medicationsPrescribed}
Follow-up Instructions: {followUp}
Referrals: {referrals}
Additional Notes
{additionalNotes}
{#diagnoses}
Diagnoses
- {code}: {description}
{/diagnoses}
{#procedures}
Procedures Performed This Visit
- {name}: {details}
{/procedures}
Signature
Provider: {clinicianName}, {clinicianTitle}
Date Signed: {signatureDate}
This document template includes dynamic placeholders for automated document generation with Documentero.com. Word Template - Free download
Download Word Template (.DOCX)Customize Template
Download the Clinical Progress Notes template in .DOCX format. Customize it to suit your needs using your preferred editor (Word, Google Docs...).
Upload & Configure
Upload the template to Documentero - Document Generation Service, then map and configure template fields for your automated workflow.
Generate Documents
Populate templates with your data and generate Word (DOCX) or PDF documents using data collected from shareable web Forms, APIs, or Integrations.
Use Cases
Automate Clinical Progress Notes Using Forms
Generate Clinical Progress Notes Using APIs
Integrations / Automations
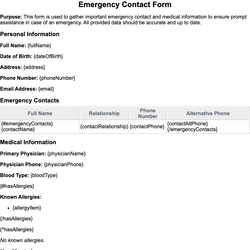
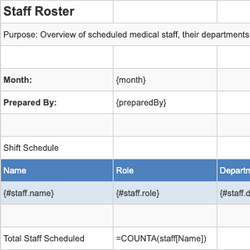
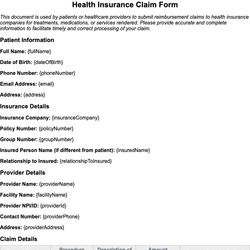
Other templates in Healthcare & Medical
DocumentDOCX
SpreadsheetXLSX
DocumentDOCX
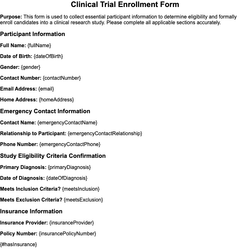
Clinical Trial Enrollment Form
DocumentDOCX